This paper is shared here for educational and archival purposes.
Hypnosis in Mind and Body
John F. Kihlstrom
University of California, Berkeley
Note: Plenary address presented to the annual meeting of the Society for Clinical and Experimental Hypnosis, Berkeley, California, October 4, 2013.
This paper honors Dr. Dabney Ewin, Clinical Professor of Surgery and Psychiatry at Tulane University Medical School, whose clinical work using hypnosis inspired me to take psychosomatics seriously. Any clinician interested in using hypnosis in treatment would profit from Dr. Ewin’s little book, 101 Things I Wish I’d Known When I Started Using Hypnosis (Crown House Publishing, 2009).
Thank you for your kind introduction. It’s always a special privilege to speak before this group.
In fact, this occasion sent my thoughts reaching back to my very first SCEH meeting, which was my very first scientific conference. It was 1970, my first year at graduate school, in Philadelphia: Martin Orne organized the local arrangements, and Fred Evans was co-chair (with Erik Wright) of the scientific program. I didn’t present any research — I had only just begun working with Martin, and Fred, and Emily Orne, and even though we had results from our first study of temporal organization during posthypnotic amnesia, the Scientific Program had been set long before. But everybody in Martin’s lab was seconded to help out at the meeting, so I did get to be present for the whole thing.
And what a meeting it was! The research workshop lasted three whole days. The scientific program began, as it always did in those days, with clinical research. Andre Weitzenhoffer discussed the “hypnotic stare”, and Herb Spiegel introduced his eye-roll sign for hypnotizability. Robert W. White, who had been Martin’s dissertation advisor, reflected on the implications of hypnosis for personality, motivation, and social interaction. Perry London discussed the prospects for increasing hypnotizability through EEG alpha training. There was a symposium on antisocial behavior and hypnosis. Ted Barber offered his “new” conceptualization of hypnosis (which turned out to look awfully like the old one). Throughout it all, there was Paul Sacerdote and Erika Fromm in the front row during the research reports, and Jack Hilgard and Ron Shor in the front row during the clinical papers. Clinicians and experimentalists together, just as it says in the name of our Society and the title of our Journal.
OK, I’ll admit it: I had to look some of those details up. But one memory especially has stuck with me, over all these years: the Presidential Banquet at the University of Pennsylvania Museum, one of the best archeological museums in the world; cocktail hour in the Chinese Rotunda, surrounding the famous crystal ball, 55 pounds of transparent quartz; dinner in the Egyptian Room, surrounded by mummies (steaks grilled on hibachis). Leston Havens, the great historian of psychiatry, talking about the connection between hypnosis and hysteria. Did I mention it was Halloween weekend? Was that David Rosenhan or Phil Zimbardo dressed in a magician’s cape, cane, and top hat? I don’t remember those details anymore. But what I do remember was that as soon as the festivities began, the Museum staff told Martin that the cash bar was strictly illegal: this was Pennsylvania, and there was no selling alcohol without a state license. So the bar had to be closed — except that Bernard Raginsky pulled out his checkbook and covered the whole expense. A great metaphor for the commitment of individual members to the good of the Society as a whole.
In my time with you today I want to return to my first point, the relation between science and practice, and discuss a new frontier for research in which scientists and practitioners can collaborate, using hypnosis to expand our understanding of the relations between mind and body.
Across the history of psychology and psychiatry, researchers of many different theoretical stripes have found hypnosis intrinsically interesting. And who wouldn’t be interested in hypnosis? Hypnotic subjects appear to lose control over voluntary motor activities; they don’t feel pain or touch, they go deaf or blind; they hear voices that aren’t there speaking to them, and they fail to see things that are right there in front of them; they feel like they’re children again; they don’t recognize objects that should be familiar to them; they come out of hypnosis unable to remember what they did while they were hypnotized; and when the experimenter gives a pre-arranged cue, they carry out some activity that had been suggested to them earlier, without knowing what they’re doing or why. Hypnosis is one of the few things you can do in a laboratory that both experimenter and subject find enjoyable — at least if the subject is highly hypnotizable; and even if he’s not, it’s still a pleasant way to pass the time.
Sometimes, as in the pioneering research of P.C. Young, hypnosis was just a phenomenon to be studied with the laboratory methods of the then-new science of psychology — the goal being to find out just what hypnosis can do and what it cannot (Young, 1925, 1926a, 1926b, 1927, 1931). This was also the view of Clark L. Hull, who simply assumed that hypnosis was a “habit phenomenon”, something that the subject got better at with practice, and who deployed his sophisticated experimental methods to study hypnosis for its own sake (Hull, 1933) — a project he abandoned in mid-course, leaving a legacy of not 100, not 101, but 102 studies of hypnosis (Hull, 1930a, 1930b), and another 40 studies on nonhypnotic suggestibility (Hull, 1929), most of which remain undone to this day (and still worth doing, hint, hint) . In much the same way, I think it’s fair to say that the “Golden Age” of modern hypnosis research, beginning in the 1950s and running into the 90s, was primarily concerned with applying established paradigms and theories to the understanding of hypnotic phenomena. Jack Hilgard and Martin Orne, Ted Sarbin and Ted Barber, and their progeny — they had theories, for sure, but mostly they had methods to match their curiosity about an intrinsically interesting phenomenon.
But this project, of understanding hypnosis in terms of what is already known, has coexisted with another project, which is to study hypnosis for the unique light it can shed on mind and behavior. This has an even longer history, extending to the clinical work of Charcot and Janet, where hypnosis served as a kind of laboratory model for understanding the mysteries of hysteria (Kihlstrom, 1979).
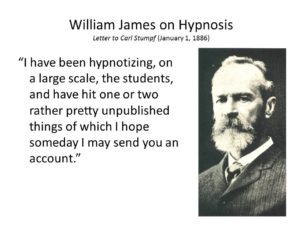
William James devoted an entire chapter of his Principles (James, 1890/1980) to hypnosis precisely because he thought the new scientific psychology could benefit from the insights it provided (Kihlstrom & McConkey, 1990). James’s interest in hypnosis had its origins in his interest in the will, and he thought that hypnosis could shed unique light on a basic problem in psychology: how ideas, in the form of suggestions, generated action, in the form of hypnotic behaviors. And, of course, James was interested in consciousness. He thought that consciousness and thinking were identical, and that unconscious thought was a kind of oxymoron; still, he was persuaded by Janet’s observations, and his own, that in hypnosis things could be unconsciously felt but not consciously perceived, and that mental activity could be divided into multiple streams, only one of which was accessible to phenomenal awareness at any given time.
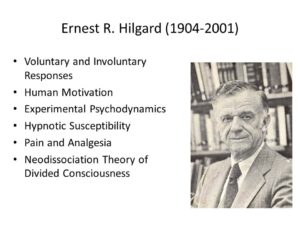
Both views — the relevance of hypnosis to motivation, and to consciousness — were carried into the work of Jack Hilgard. At first, Hilgard’s interest in hypnosis was carried over from his early work on learning, and especially the distinction between voluntary and involuntary responses (Hilgard, 1948; Hilgard & Marquis, 1940). Like James, he thought that hypnosis was relevant to motivation, and especially the translation of ideas into action. His own program of research had its origins in his interest in psychodynamic theory, and the idea that behavior could arise from unconscious ideas and motives (Hilgard, 1952, 1961). Finally, the relevance to consciousness was expressed most clearly in his “neodissociation” theory of divided consciousness (Hilgard, 1977).
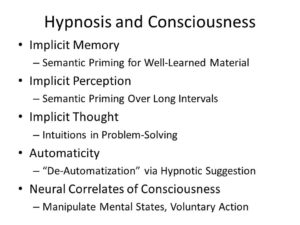
Over the years, hypnosis has offered much to psychological theory, and particularly to our understanding of consciousness (Kihlstrom, 2007, 2013). Studies of posthypnotic amnesia, hypnotic blindness, for example, offer a new perspective on unconscious memory and perception. Most studies of implicit memory require relatively impoverished encoding conditions, and are limited to what is known as repetition priming — which, frankly, is not a very interesting form of memory. But with hypnosis we can get semantic priming even for well-learned material. This shows us that unconscious memory can occur even with richly elaborated, organized material. Similarly, most studies of implicit perception degrade the stimulus through such techniques as masking, which effectively preclude the subject from analyzing the stimulus effectively, so that when you get semantic priming, it’s analytically limited and doesn’t last very long. Not so in hypnotic blindness and deafness — which, again, indicates that unconscious perception can occur even when the subject can devote full attentional resources to processing the stimulus. Kenneth Bowers’ seminal studies of intuition, which shed new on the nature and scope of unconscious thinking, were directly inspired by his earlier studies of posthypnotic suggestion. And then, finally, we have recent studies of the effects of hypnotic agnosia on performance on the Stroop task — which indicate that mental processes, once automatized and rendered unconscious, can be de-automatized and performed consciously.
And that’s not all. Hypnosis has also made important contributions to theory in personality and social psychology, developmental psychology, and, of course, clinical psychology.
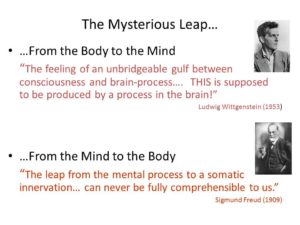
I won’t detail these further, because I want to dwell for a considerable amount of time on what I think is a new frontier for hypnosis research, which allies both scientists and practitioners: psychosomatic medicine, a field predicated on the idea that patients’ feelings and beliefs can affect the functioning of their bodies (Harrington, 2008). This reveals another side of the mind-body problem. Ever since Descartes, science has been consumed by the question of how, or even whether, mental states are produced by bodily processes — a problem which is now generally known as the neural correlates of consciousness. But in psychosomatics, we’re interested in the reverse: whether, and if so how, mental states affect bodily processes.
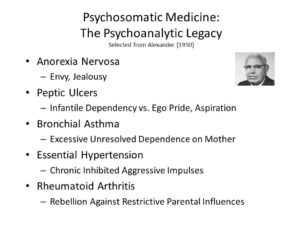
Now, psychosomatic medicine is in bad odor in psychiatry and clinical psychology these days — in part, to be honest, because of the excesses of psychoanalytic theory, which held, among other things, that bronchial asthma was caused by excessive unresolved dependence on one’s mother (Alexander, 1950).

But much of the blame also falls on the biological revolution in psychiatry, and the general reluctance of most physicians, even psychiatrists, to take psychosocial processes seriously. Consider, for example, the proclivity of so many mental-health professionals to dispense medication to their depressed and anxious patients, and the reluctance of insurance companies to pay for much by way of psychotherapy — even under health care reform. I have remarked elsewhere that the ideal to which many physicians seem to aspire is the “feinberger” (or medical “tricorder”) and surgical bio-bed used by Dr. McCoy in the Star Trek series, which permitted the diagnosis and treatment of illness without speaking to or touching the patient (Kihlstrom, 2003, 2008). Too many physicians appear to be threatened by the notion that the physical state of their patients could be affected by the mental state of their patients, and they’d like to get rid of psychosomatics by whatever means necessary. Present company excepted, of course: hypnosis teaches us to talk, and listen, to our patients.
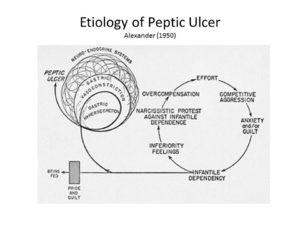 As a case in point, consider the status of stomach ulcers. The traditional psychoanalytic formulation is that peptic ulcers arise from an unconscious conflict between infantile dependency and ego pride (Alexander, 1950).
As a case in point, consider the status of stomach ulcers. The traditional psychoanalytic formulation is that peptic ulcers arise from an unconscious conflict between infantile dependency and ego pride (Alexander, 1950).
It’s easy to make fun of such proposals now, but — as Susan Sontag reminded us in Illness as Metaphor (1978), it was not that long ago that psychiatrists proposed that cancer was itself psychosomatic, caused by people who bottled their emotions up so tightly that they burst forth as tumors.
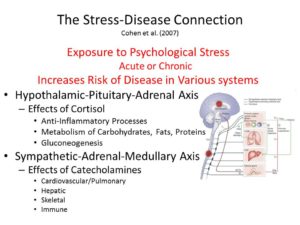
A more recent view implicates stress of any kind, mediated through the “flight or fight” reaction. As such, it exemplifies what we can call the stress-disease connection (Cohen, Janicki-Deverts, & Miller, 2007) mediated by the hypothalamic-pituitary-adrenocortical axis (HPA) or the sympathetic-adrenal-medullary axis (SAM).
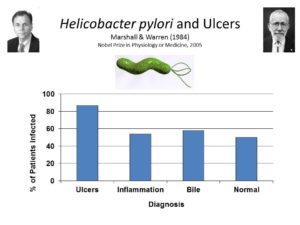
Both views were challenged by discovery, in the 1980s, of an association between peptic ulcers and infection with a bacterium known as helicobacter pylori — work that won the 2005 Nobel Prize in Physiology or Medicine for Barry Marshall and Robin Warren (Marshall & Warren, 1984).
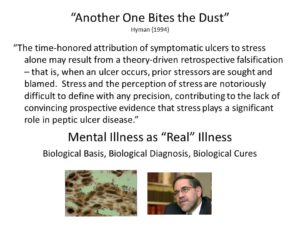 After Marshall and Warren published their discovery, Steven Hyman, a leading molecular neuropsychiatrist, soon to become the Director of the National Institute of Mental Health, later Provost of Harvard University, and currently the Director of the Stanley Center for Psychiatric Research at Harvard and MIT, wrote a commentary entitled “Another One Bites the Dust” celebrating the triumph of biomedicine over psychology (Hyman, 1994).
After Marshall and Warren published their discovery, Steven Hyman, a leading molecular neuropsychiatrist, soon to become the Director of the National Institute of Mental Health, later Provost of Harvard University, and currently the Director of the Stanley Center for Psychiatric Research at Harvard and MIT, wrote a commentary entitled “Another One Bites the Dust” celebrating the triumph of biomedicine over psychology (Hyman, 1994).
Hyman’s paper epitomizes the biological and pharmacological revolution in mental health. The same attitude is reflected in a famous aphorism attributed to Ralph Gerard, founder of the Society for Neuroscience, that “behind every twisted thought there lies a twisted molecule” (Healy, 2004). And, more recently, in the promise of Thomas Insel, the current Director of the National Institute of Mental Health, that the key to mental illness will be found in the Human Connectome, rather than in any analysis of human experience, thought, and action (Insel, 2010).
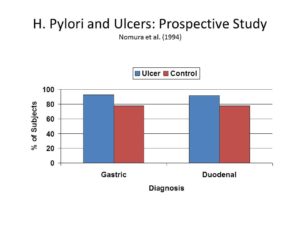 But not so fast. It turns out that, while antibodies for H. pylori infection are found in over 90% of ulcer patients, they are also found in almost 80% of ulcer-free patients, leading one group of researchers to conclude that “other factors in addition to H. pylori infection have an important role in the development of peptic ulcer” (Nomura, Stemmermann, Chyou, Perez-Perez, & Blaser, 1994).
But not so fast. It turns out that, while antibodies for H. pylori infection are found in over 90% of ulcer patients, they are also found in almost 80% of ulcer-free patients, leading one group of researchers to conclude that “other factors in addition to H. pylori infection have an important role in the development of peptic ulcer” (Nomura, Stemmermann, Chyou, Perez-Perez, & Blaser, 1994).
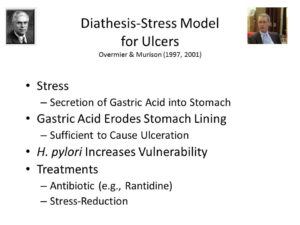
Moreover, Bruce Overmier and Robert Murison have developed an animal model of ulcers which clearly shows that stress, in the form of unpredictable and uncontrollable foot shock, clearly “precipitates and sustains” gastric ulceration (Overmier & Murison, 2013). In their model, h. pylori may increase vulnerability to gastric secretions, but it is not their sole cause. The effects of stress on the body may be mediated by the HPA and SAM, in physiological terms, but stress is fundamentally a mental state, involving the organism’s perception of environmental challenges.
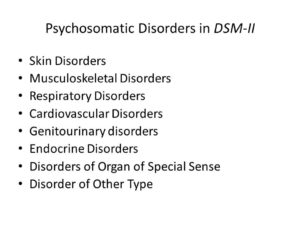
The evolution of the Diagnostic and Statistical Manual of Mental Disorders (DSM) also illustrates the problem. The first two editions of DSM, published in 1952 and 1968, respectively, listed the psychosomatic disorders in their own special section — perhaps owing to the influence of psychoanalysis.
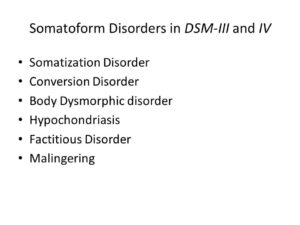
But the entire category was dropped in DSM-III, essentially relegating the psychosomatic disorders to a footnote. In this respect, at least, the later editions of DSM made a big mistake, creating a diagnostic category that — to adopt the language of Kurt Vonnegut (in Cat’s Cradle, 1963) — is more a granfaloon than a karass In the first place, the conversion disorders reflect pseudoneurological problems with specific aspects of consciousness, either conscious awareness of sensations and percepts or conscious control of motor function, and properly belong with the dissociative disorders (Kihlstrom, 1994). The somatoform disorders, including somatization disorder and hypochondriasis, are instances where the patient has multiple unexplained physical complaints that really serve to communicate emotional distress, or to manipulate other people (Kihlstrom & Canter Kihlstrom, 1999). The complaints are medically unexplained, meaning that physical examination and diagnostic testing reveals that there’s nothing wrong with the body. But in the psychosomatic disorders there is definitely something wrong with some specific bodily function: in ulcers, for example, there are those nasty lesions in the lining of the small intestine and the stomach. They’re not just somatoform — they’re somatic for real. And they don’t just “contribute” to the patient’s medical condition: They cause it to begin with.
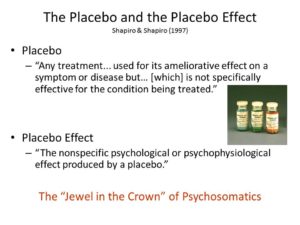
And finally, there is the placebo effect — sometimes called the “crown jewel” of psychosomatic medicine, because it reveals the effects of mental states — attitudes, beliefs, and expectations, feelings and motives — on physical outcomes (Beecher, 1955; Harrington, 1997; Shapiro & Shapiro, 1997). Note, first, that the clinical trials that validate new drugs, devices, or procedures virtually mandate a comparison to placebo. The implication is that placebo effects are something to be done away with, rather than capitalized on.
Placebo effects themselves aren’t of substantive interest, which is why Hrobjartsson and Gotszche were able to find only 114 studies in the whole medical literature that compared placebo to a no-treatment control (Hrobjartsson & Gotzsche, 2001a, 2001b). And, of course, for all the attention paid to placebo effects in both the popular and professional press, these authors — perhaps with relief, perhaps with glee — found scant evidence of a placebo effect on any biological endpoint, such as nausea, asthma, or hypertension. Placebos may make people feel better — though, frankly, Hrobjartsson and Goetsche doubt even that; but they don’t seem to actually get better. This is a real challenge for placebo research — to show that placebos and other psychological interventions can have an effect on somatic functioning (Price, Finniss, & Benedetti, 2008).
Let me be clearer about what I mean — and you’ll have to pardon the dualism in what I’m about to say. After all, I’m a psychologist, and psychology is essentially dualistic in nature: as William James (James, 1890/1980) (p. 1) understood. Psychology is the science of mental life, and we can do our work at the psychological level of analysis without ever asking how the brain does it. That’s a different level of analysis, and while the neural basis of mental life is interesting, psychologists are under no obligation to study it. “Neodualists” like myself acknowledge that the mind has its biological basis in the brain, but insist that mental life can be analyzed at its own level, without reduction to biology or physics. Or, as Ulric Neisser famously put it, psychology isn’t “just something to do until the biochemist comes” (Neisser, 1967) (p. 1).
Anyway, placebo and other psychosomatic effects have their origins in the person’s mental state — his or her knowledge or beliefs, attitudes and expectancies, feelings and drives. The best-documented placebo effects, undoubted even by Hrobjartsson and Gotszche, are in the domains of pain and depression. As Fred Evans (Evans, 1974) and others have shown, big, dark-colored, bad-tasting, expensive placebos are more effective than small, brightly colored, good-tasting, discounted ones; placebos delivered intravenously are more powerful than those delivered intramuscularly or orally; and, beautifully, the magnitude of the placebo effect is a constant proportion of the active agent to which it is being compared (roughly 55%). And as Irving Kirsch famously found, the bulk of the effect of most antidepressant drugs currently on the market is accounted for by placebo effects (Kirsch, Moore, Scoboria, & Nicholls, 2002). The same is probably true for anxiolytics. But pain, depression, and anxiety are mental states, and they don’t count as psychosomatic effects. To count as psychosomatic, we have to have evidence that suggestion and belief influence actual bodily functioning.
But that’s not all we have to show, because every mental state is associated with some neural state — even diehard dualists acknowledge this, as in Leibnitz’s doctrine of psychophysical parallelism. In that sense, we’re all materialists now, even if we don’t have a complete grasp of how brain states cause mental states — and even if we prefer to confine our research and theories to the psychological level of analysis. So, when a brain-imaging study finds that hypnotic analgesia is associated with changes in the somatosensory cortex or the anterior cingulate gyrus (Rainville, Hofbauer, Bushnell, Duncan, & Price, 2002), or that hypnotic color blindness is associated with changes in area V4 of extra-striate cortex (Kosslyn, Thompson, Costantini-Ferrando, Alpert, & Spiegel, 2000), that should surprise nobody — except those who think that hypnotic subjects don’t really experience subjectively compelling changes in perception. Any change in mental state must be associated with a change in brain state, for the simple reason that “the mind is what the brain does” (Minsky, 1987).
So if we really want to demonstrate psychosomatic effects, we’ve got to get out of the nervous system, and into other systems of the body — like the gastrointestinal system, in the case of psychosomatic ulcers. And here’s where hypnosis comes in, because we have a long history of obtaining such effects with hypnosis (Black, 1969; Bowers & Kelly, 1979; Covino, 2008; Covino & Pinnell, 2010; Johnson, 1989).
Perhaps the “mother” of all such studies is the famous case, reported by A.A. Mason, of a 16-year-old boy suffering from congenital icthyosiform erythrodermia of Broq (Mason, 1952, 1955). This is a hereditary disorder affecting the skin, which becomes discolored and blackened, horny, inelastic, fissured, and peppered with vascular protuberances. Conventional treatment, including skin grafts from unaffected portions of the body, failed. As a last resort, Mason hypnotized the patient, and suggested that the lesions would disappear — first from one arm, then the other, then the two legs each in turn, and finally the trunk. The progressive remission of the lesions, highly correlated with the suggestions, was documented photographically both at the end of treatment and at a four-year followup.
At these meetings in 2007, Mason reported that he subsequently saw eight more cases like this, and hypnosis didn’t work with any of them. But positive results have been obtained in other conditions. Just a couple of highlights: these are mostly old studies, but they are very provocative, so let me remind you of some of this history.
Some of these cases involved the Mantoux reaction, a diagnostic skin test for tuberculosis. In another classic of the hypnosis literature, Stephen Black gave four Mantoux-positive patients, all of whom were known to be highly hypnotizable, suggestion decreased the size of both the swelling and the hardened area (Black, Humphrey, & Niven, 1963). Interestingly, a biopsy showed that the underlying histology was unchanged; but, objectively, the swelling and hardness did go down.
There have also been positive results with allergic reactions. In one case of a pollen allergy that had resisted treatment for 10 years, Mason and Black found that, after suggestion, the patient showed no hypersensitivity to injected allergens (Mason & Black, 1958). In a followup, Black tested 12 more patients, and obtained positive results with six of the seven who were highly hypnotizable, and two of four who were moderately hypnotizable (Black, 1963). Much as with the Mantoux study, however, while the skin reaction was inhibited, the Prausnitz-Kustner reaction indicated that the underlying serology was unchanged.
In yet another classic study, Yujiro Ikemi and Shunji Nakagawa employed a variant on the symptom-provocation method to study the effects of suggestion on a form of contact dermatitis, similar to poison ivy or poison oak, induced by skin contact with the leaves of the lacquer and wax trees common in Japan and other parts of East Asia (Ikemi & Nakagawa, 1962). In their study, 13 male high-school students, known to be sensitive to these leaves, were blindfolded. When they were actually brushed with the poisonous leaves, but told the leaves were from the harmless chestnut tree, 11 subjects showed reduced signs of dermatitis. When they were touched with the chestnut-tree leaves, but told they were being touched with poisonous leaves, all 13 showed signs of dermatitis. When the same procedure was applied to another group of students, who had never experienced an allergic reaction to the poisonous trees, there was little response to the suggestions either way.
Finally, a clinical series by David Collison (1975) included a large number of allergic patients seen over a 10-year period. Dr. Collision did not use a formal measure of hypnotizability, but he did make a clinical assessment of the “depth” of hypnosis his patients attained during treatment, which for my purposes can serve as a proxy for hypnotizability. Fully 19 of 43 hypnotizable patients showed complete remission, and another 17 improved; six of 47 mediums were cured, and only 21 improved; none of 31 insusceptible patients were cured, though two did show improvement following suggestion.
All of these are clinical studies, and lack the kind of experimental controls that we’d need to really pin down these effects. We’d like to see better assessments of hypnotizability, for example, and we’d also like to see a placebo condition. I say this because some theorists seem inclined to identify the effects of hypnosis with placebo effects. This is a mistake on at least two counts. First, as I indicated earlier, placebo effects are things that many clinicians (and researchers) want to get rid of, and we don’t want to throw the hypnotic baby out with the placebic bathwater. Second, identifying hypnosis with placebos obscures the fact that hypnosis is, itself, an active therapeutic agent — just like a drug or a pacemaker, surgery or psychotherapy. This is true even in the case of pain, where placebo effects are arguably the strongest (Evans & McGlashan, 1987; McGlashan, Evans, & Orne, 1969).
In recent correspondence, Dr. Dabney Ewin has reminded me that Mason’s case of icthyosis was originally misdiagnosed as a particularly bad one of warts. And, in fact, it was this initial misdiagnosis that led Mason to try hypnosis in the first place. He knew that hypnosis had a long history as an effective treatment for warts, so he gave it a shot. If he had known that the patient’s disease was hereditary, he might never even have tried. So let’s look at hypnosis and warts for a moment. The first such study to come to mind, of course, is Dr. Ewin’s own report of success in 80% of 41 consecutive cases (Ewin, 1992). Of course, warts also remit spontaneously, so we’d like to see some additional controls.
In a pioneering study, Asher (1956) reported the results of 33 consecutive patients treated for multiple warts, with cures in 11 of 17 hypnotizable patients but none of 8 insusceptible patients. Ullman and Dudek got a similar, if less dramatic difference between hypnotizable and insusceptible patients, so there’s something going on here besides mere spontaneous regression. Sinclair-Gieben and Chalmers (1959) treated 14 patients with bilateral warts with hypnotic suggestions that targeted only one side of the body. On 3-month followup, all 9 hypnotizable patients showed remission of the warts, but only on the targeted side of the body; the 5 insusceptible subjects showed no changes on either side. Again, this study has a nice control for spontaneous remission: the untreated side. Unfortunately, a replication by Surman and colleagues found no difference between treated and untreated sides, although they did report some improvement in 9 of 17 patients given suggestions, compared to none of 7 patients in an untreated wait-list control condition (Surman, Gottlieb, Hackett, & Silverberg, 1973).
The first investigators to bring this problem into the laboratory were Richard Johnson and Ted Barber, who got a markedly lower success rate: only 3 of 11 subjects given hypnotic suggestions showed remission of their warts. But then again, none of the 11 subjects given the same suggestions without hypnosis showed any improvement at all (Johnson, 1989). It’s unfortunate that Johnson and Barber didn’t classify their subjects according to hypnotizability — though not particularly surprising, given Barber’s theoretical orientation at the time In fact, I believe that it was this study that prompted a turn in Ted’s theorizing, toward a view that hypnosis might have some special properties after all (Barber, 1999, 2000).
Nick Spanos and his colleagues also attacked the problem of warts, and with results that must have surprised them, too (Spanos, Stenstrom, & Johnson, 1988). Reasoning that hypnosis might work by virtue of the myths and urban legends surrounding it, they included a plausible placebo control in the form of a “cold laser” machine for wart removal, as well as an untreated control group. Only hypnosis led to a significant reduction in warts.
A second study employed four groups, and got comparable effects when subjects received a nonhypnotic suggestion, leading the authors to conclude that the operative factor was the suggestion, not hypnosis — a point to which I’ll return later.
In a later study, hypnosis proved superior to a common over-the-counter medical treatment, the topical application of salicylic acid, as well as a topical placebo (Spanos, Williams, & Gwynn, 1990). It would be very interesting to see a similar study comparing hypnosis with liquid nitrogen cryotherapy, which is the current standard of care.
There are lots more studies of warts, but the ones that I’ve cited make the point convincingly: there just might be something interesting going on here: the hypnotist’s suggestion is having an effect on a physiological process that lies outside the brain and central nervous system. Note, too, that these studies arise, first, in the clinic — and then are brought into the laboratory for systematic controlled investigation. There are a still a lot of questions that have to be answered. To illustrate, let’s follow the warts example a little further.
First, of course, we need to nail down any effects definitively, by including placebo and untreated control groups — and, for that matter, comparisons to the standard of care. It may be, for example, that hypnosis can’t match the outcomes achieved with the standard of care — whether that is salicylic acid or liquid nitrogen. But it might be useful when, for whatever reason, the standard medical treatment is inappropriate.
At the same time, the combination of hypnosis with the standard of care may be particularly effective — much as the combination of drugs with psychotherapy is particularly potent with depression. Alternatively, it may be that standard medical treatment is better at immediate symptom relief, but hypnosis is better at maintaining remission. Liquid nitrogen might get rid of warts fairly quickly, but hypnosis might keep them away.
We need clarification on the role of hypnotizability in moderating these effects. By definition, any effect of hypnosis ought to be correlated with hypnotizability. There are hints in the clinical studies of warts that this might be the case — though, unfortunately, the laboratory studies failed to classify subjects for hypnotizability.
On the other hand, we should also compare hypnosis with nonhypnotic suggestion. In one of his studies, Spanos got comparable effects without inducing hypnosis. Here again, hypnotizability may be an issue. In the case of skin allergy, for example, Ikema and Nakazawa got their effects regardless of whether they used hypnosis — so long as the subjects themselves were hypnotizable.
Then we need to know how “deep” these effects go. None of the warts studies have done anything more than count the number of warts visible before and after treatment. But warts are caused by one or another form of the human papilloma virus (HPV): there may be hundreds of these, though apparently only a small number are clinically important. We’d like to know whether there are effects on the HPV virus itself. Recall that, in his studies, Black found that hypnotic suggestion modified the expression of the Mantoux reaction on the surface of the skin, but not the underlying histology. On the other hand, his suggestion didn’t target the underlying histology — only the visible surface of the skin.
And how broad are these effects? Most studies of warts target common cutaneous warts, caused by HPV Types 2 and 4, which are benign if annoying. But what about the more troublesome plantar warts, which are caused by a different strain of HPV, Type 1? Or something more serious, like genital warts, caused by HPV 6 and 11? Even in this age of Gardasil, there are as many as a million new cases of genital each year. Can we get rid of those warts as well? Can we prevent them from coming back? What are the effects of hypnotic treatment on the risk for cervical cancer?
In this regard, Arreed and Marianne Barabasz and their colleagues published a very promising study comparing hypnosis with standard medical treatments, which included topical Imiquimod (which is directed at the immune response), cryotherapy, or surgical removal (Barabasz, Higley, Christensen, & Barabasz, 2010). The study did not employ random assignment to conditions, but even so hypnosis did as well as conventional treatment, even at 12-week followup.
This is an area of research in which clinicians and experimentalists can collaborate as equals, in a way that benefits both constituencies. In some respects, our clinical colleagues are way ahead of the experimentalists — trying hypnosis to see whether it works. On the other hand, controlled laboratory research will promote clinical utilization, by giving skeptical colleagues a reason to try hypnosis for themselves — and third parties a reason to pay for it.
One area of potential application, relatively unstudied, is burns (Patterson, Goldberg, & Ehde, 1996). Again, I think of Dabney Ewin’s remarkable case study of a boy who was burned by boiling cooking fat (Ewin, 1986). And there are some controlled experiments, too, which raise further questions about the mechanics of these effects. In a classic study, Chapman, Goodell, and Wolff found that targeted suggestions decreased inflammation in experimentally induced bilateral burns (Chapman, Goodell, & Wolff, 1959a, 1959b). They also found that the suggestion of a burn increased skin temperature (Hammond, Keye, & Grant, 1983). There are also some clinical studies, which raise additional questions of mechanism (Margolis, Domangue, Ehleben, & Shrier, 1983; Moore & Kaplan, 1983). For example, how much of the healing is a side effect of suggested analgesia? What are the effects of suggestions for cooling of the skin in the affected area, or increased blood flow?
Similar studies could be done in the area of wound-healing, whether the wounds are surgically induced or a product of misadventure. Ginandes and her colleagues found that adjunctive hypnosis accelerated healing after reduction mammoplasty (Ginandes, Brooks, Sando, Jones, & Aker, 2003). Compared to a group who received the surgical standard of care, patients who received adjunctive hypnosis showed faster wound healing over 7 weeks post-surgery. These same authors had earlier found similar effects on the healing of bone fractures, which offers another area for clinical research (Ginandes & Rosenthal., 1999). Again, we’d like to know how much of these effects are due to direct suggestion, and how much to relaxation and stress-reduction.
There are many more studies along these lines. Most of them are old, many of them are small in scope, and some do not come up to contemporary standards for either clinical or experimental research. But I’ve reviewed them here because they constitute a legacy of hypnosis that has been largely forgotten or ignored — a legacy that still holds considerable potential value for both clinical practice and basic theory.
On the practical side, they suggest that hypnosis has the potential to be an important treatment modality in a wide variety of medical contexts — not just in psychotherapy, or for the relief of pain. Now, I don’t want to oversell these effects. Nobody treating cancer should abandon surgery, radiation, or chemotherapy in favor of hypnosis. But it seems likely that hypnosis has a place in the active treatment of a wide variety of medical conditions, especially as an adjunct to standard medical treatments. The use of hypnosis in the pain clinic may be a model here. For example, Elvira Lang and her associates have shown clearly that adjunctive hypnosis can reduce requests for conscious sedation in outpatient surgery, and it’s cost-effective as well! (Lang et al., 2000). (A distraction condition also reduced medication use, but hypnosis had other advantages that aren’t shown here.) More results like that should enhance the appeal of hypnosis to both service providers and third-party payers.
But even if the effects of hypnosis on bodily functions are not substantial or reliable enough to be of routine clinical use, they’re still of great potential theoretical importance, because of their relevance to the mind-body problem — that great unsolved problem in philosophy and psychology. There are, actually four mind-body problems, quite different from each other.
First, there is the standard mind-body problem, which has to do with the biological substrates of mental life. Here we are dealing with the neural correlates of consciousness — the causal link between brain states and mental states. What is going on in the brain when we perceive an object, remember an event, or contemplate an idea? What are the neural differences between conscious and unconscious perception, memory, and thought? And also the problem of embodied cognition — how do other bodily states, such as those involved in emotion and motivation, affect perception, memory, and thought?
Second, there is the question of body without mind — perhaps bringing up images of Hollywood zombies, who lack conscious awareness and control. How much of our behavior occurs independently of any conscious mental processes at all? How much is just plain reflex or instinct? How much is automatic, executed outside of conscious awareness and without any conscious intention?
Third, the question of mind without body. Does mental life exist in the absence of any physical substrate at all? In the 19th century, this was the domain of spiritualism. In the 20th and 21st centuries, we call it parapsychology, the out-of-body experience, or the near-death experience.
And last, but not least, the problem that has been my topic today: how mind influences body — how beliefs, attitudes, ideas, and other thoughts can influence bodily states and processes. This is the theoretical relevance of psychosomatics, and it is here where hypnosis can make a great, I think unique, contribution, because they take us beyond the stress-disease connection. It’s one thing for stress to cause disease through activation of the autonomic nervous system, the HPA and SMA, and all that, as in the case of cardiovascular disease, ulcers, and other conditions. It’s one thing for relaxation, meditation, and other stress-reduction techniques to help reverse these stress-related conditions. It’s quite another thing for a patient’s belief that he is in contact with a poisonous plant leaf to give rise to an eruption of dermatitis, or for a suggestion that warts will disappear to lead to their actual disappearance.
Now, with further research it may turn out that hypnosis isn’t necessary to produce these effects, or even high hypnotizability. It doesn’t really matter. We’d never find out about these psychosomatic relationships except for the inspiration that came from hypnosis research. In that way, hypnosis will once again lead the way to discovering something new about mind and body.
Thank you very much. Welcome to Berkeley, and have an enjoyable meeting.
References
Alexander, F. (1950). Psychosomatic medicine: Its principles and applications. New York: Norton.
Barabasz, A., Higley, L., Christensen, C., & Barabasz, M. (2010). Efficacy of hypnosis in the tretament of human papillomavirus (HPV) in women: Rural and urban samples. International Journal of Clinical & Experimental Hypnosis, 58(1), 102-121.
Barber, T. X. (1999). Hypnosis: A mature view. Contemporary Hypnosis, 16, 123-127.
Barber, T. X. (2000). A deeper understanding of hypnosis: Its secrets, its nature, its essence. AMERICAN JOURNAL OF CLINICAL HYPNOSIS, 42(3-4), 208-272.
Beecher, H. K. (1955). The powerful placebo. Journal of the American Medical Association, 159, 1602-1606.
Black, S. (1963). Inhibition of immediate-type hypersensitivity response by direct suggestion under hypnosis. British Medical Journal(June 22), 925.
Black, s. (1969). Mind and body. London: Kimber.
Black, S., Humphrey, H. H., & Niven, J. S. F. (1963). Inhibition of Mantoux Reaction by direct suggestion under hypnosis. Brit. med. J., 5346, 1649-1652.
Bowers, K. S., & Kelly, P. (1979). Stress, disease, psychotherapy, and hypnosis. Journal of Abnormal Psychology, 88, 506-526.
Chapman, L. F., Goodell, H., & Wolff, H. G. (1959a). Augmentation of the inflammatory reaction by activity of the central nervous system. AMA Archives of Neurology, 1(5), 557-572.
Chapman, L. F., Goodell, H., & Wolff, H. G. (1959b). Changes in tissue vulnerability induced during hypnotic suggestion. Journal of Psychosomatic Research, 4, 99-105.
Cohen, S., Janicki-Deverts, D., & Miller, G. E. (2007). Psychological stress and disease. Journal of the American Medical Association, 298, 1685-1687.
Covino, N. A. (2008). Medical illnesses, conditions and procedures. In M. R. Nash & A. J. Barnier (Eds.), Oxford handbook of hypnosis: Theory, research, and practice (pp. 611-624). Oxford: Oxford University Press.
Covino, N. A., & Pinnell, C. M. (2010). Hypnosis and medicine. In s. J. Lynn, J. W. Rhue & I. Kirsch (Eds.), Handbook of clinical hypnosis (pp. 551-573). Washington, d.C.: American Psychological Association.
Evans, F. J. (1974). The placebo response in pain reduction. In J. J. Bonica (Ed.), Advances in Neurology (pp. 289-296). New York: Raven.
Evans, F. J., & McGlashan, T. H. (1987). Specific and nonspecific factors in hypnotic analgesia: A reply to Wagstaff. British Journal of Experimental and Clinical Hypnosis, 4, 141-147.
Ewin, D. M. (1986). Emergency room hypnosis for the burned patient. Americal Journal of Clinical Hypnosis, 29, 7-12.
Ewin, D. M. (1992). Hypnotherapy for warts (verruca-vulgaris): 41 consecutive cases with 33 cures. American Journal of Clinical Hypnosis, 35, 1-10.
Flammer, E., & Alladin, A. (2007). The efficacy of hypnotherapy in the treatment of psychosomatic disorders: Meta-analytical evidence. International Journal of Clinical & Experimental Hypnosis, 55(3), 251-274.
Ginandes, C., Brooks, P., Sando, W., Jones, C., & Aker, J. (2003). Can Medical Hypnosis Accelerate Post-Surgical Wound Healing? Results of a Clinical Trial. American Journal of Clinical Hypnosis, 45(4), 333-352.
Ginandes, C., & Rosenthal., D. I. (1999). Using hypnosis to accelerate the healing of bone fractures: A randomized controlled pilot study. Altern Th H, 5, 67+.
Hammond, D. C., Keye, W. R., & Grant, C. W. (1983). Hypnotic analgesia with burns: An initial study. American Journal of Clinical Hypnosis, 26, 60-61.
Harrington, A. (2008). The cure within: A history of mind-body medicine. N.Y.: Norton.
Harrington, A. (Ed.). (1997). The placebo effect: An interdisciplinary exploration. Cambridge, Ma.: Harvard University Press.
Healy, D. (2004). The creation of psychopharmacology. Cambridge, Ma.: Harvard University Press.
Hilgard, E. R. (1948). Theories of learning. New York,: Appleton-Century-Crofts.
Hilgard, E. R. (1952). Experimental approaches to psychoanalysis. In E. Pumpian-Mindlin (Ed.), Psychoanalysis as science: The Hixon Lectures on the scientific status of psychoanalysis (pp. 3-45). Stanford, Ca.: Stanford University Press.
Hilgard, E. R. (1961). Hypnosis and experimental psychodynamics Lectures on experimental psychiatry (pp. 193-212). Pittsburgh, Pa.: University of Pittsburgh Press.
Hilgard, E. R. (1977). Divided consciousness: Multiple controls in human thought and action. New York: Wiley-Interscience.
Hilgard, E. R., & Marquis, D. G. (1940). Conditioning and learning. New York, London,: D. Appleton-Century Company.
Hrobjartsson, A., & Gotzsche, P. C. (2001a). Core belief in powerful effects of placebo interventions is in conflict with no evidence of important effects in a large systematic review. Advances in Mind-Body Medicine, 17, 312-318.
Hrobjartsson, A., & Gotzsche, P. C. (2001b). Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. New England Journal of Medicine, 344(21), 1594-1602.
Hull, C. L. (1929). Quantitative methods of investigating waking suggestion. Journal of Abnormal & Social Psychology, 24, 153-169.
Hull, C. L. (1930a). Quantitative methods of investigating hypnotic suggestion. Part 1. Journal of Abnormal & Social Psychology, 25, 200-223.
Hull, C. L. (1930b). Quantitative methods of investigating hypnotic suggestion. Part 2. Journal of Abnormal & Social Psychology, 25, 390-417.
Hull, C. L. (1933). Hypnosis and suggestibility: An experimental approach. New York: Appleton.
Hyman, S. E. (1994). Another one bites the dust: An infectious origin for peptic ulcers. Harvard Review of Psychiatry, 1, 294-295.
Ikemi, Y., & Nakagawa, S. (1962). A psychosomatic study of contagious dermatitis. Kyushu Journal of Medical Science, 13, 335-352ff.
nsel, T. R. (2010). Faulty circuits. Scientific American(April).
James, W. (1890/1980). Principles of Psychology. Cambridge, Ma.: Harvard University Press.
Johnson, R. F. Q. (1989). Hypnosis, suggestion, and dermatological changesL A consideration of the production and diminution of dermatological entities. In N. P. Spanos & J. F. Chaves (Eds.), Hypnosis: Cognitive-behavioral perspectives (pp. 297-312). Buffalo, N.Y.: Prometheus.
Kihlstrom, J. F. (1979). Hypnosis and psychopathology: Retrospect and prospect. Journal of Abnormal Psychology, 88(5), 459-473.
Kihlstrom, J. F. (1994). One hundred years of hysteria. In S. J. Lynn & J. W. Rhue (Eds.), Dissociation: Clinical and theoretical perspectives. (pp. 365-394). New York, NY, USA: The Guilford Press.
Kihlstrom, J. F. (2003). Expecting that a treatment will be given, when it won’t, and knowing that a treatment is being given, when it is [Commentary on “Open versus hidden medical treatments: The patient’s knowledge about a therapy affects therapy outcome” by F. Benedetti, G. Maggi, L. Lopiano, M. Lanotte, I. Rainero, S. Vighetti, & A Pollo]. Prevention & Treatment, 6, Article 4.
Kihlstrom, J. F. (2007). What hypnosis does for experimental psychology. Paper presented at the American Psychological Association, San Francisico.
Kihlstrom, J. F. (2008). Placebo: Feeling better, getting better, and the problems of mind and body. McGill Journal of Medicine, 11, 212-214.
Kihlstrom, J. F. (2013). Hypnosis and cognition. Psychology of Consciousness, submitted.
Kihlstrom, J. F., & Canter Kihlstrom, L. (1999). Self, sickness, somatization, and systems of care. In R. J. Contrada & R. D. Ashmore (Eds.), Self, social identity, and physical health: interdisciplinary explorations (Vol. 2). New York: Oxford University Press.
Kihlstrom, J. F., & McConkey, K. M. (1990). William James and hypnosis: A centennial reflection. Psychological Science, 1(3), 174-178.
Kirsch, I., Moore, T. J., Scoboria, A., & Nicholls, S. S. (2002). The emperor’s new drugs: An analysis of antidepressant medication data submitted to the US Food and Drug Administration. Prevention & Treatment, 5(Article 23).
Kosslyn, S. M., Thompson, W. L., Costantini-Ferrando, M. F., Alpert, N. M., & Spiegel, D. (2000). Hypnotic visual hallucination alters brain color processing. American Journal of Psychiatry, 157(8), 1279-1284.
Lang, E. V., Benotsch, E. G., Fick, L. J., Lutgendorf, S., Berbaum, M. L., Berbaum, K. S., . . . Spiegel, D. (2000). Adjunctive non-pharmacological analgesia for invasive medical procedures: A randomised trial. Lancet, 355(April 29), 1486-1500.
Locke, S. E., Ransil, B. J., Zachariae, R., Molay, F., Tollins, K., Covino, N. A., & Danforth, D. (1994). Effect of hypnotic suggestion on the delayed type hypersensitivity response. Journal of the American Medical Association, 272, 47-52.
Locke, S. E., Ransil, B. J., Covino, N. A., Toczydlo, J., Lohse, C. M., Dvorak, H. F., . . . Frankel, F. H. (1987). Failure of hypnotic suggestion to alter immune response to delayed type hypersensitivity antigens. Annals of the New York Academy of Sciences, 496, 745-749.
Margolis, c., Domangue, B. B., Ehleben, C., & Shrier, L. (1983). Hypnosis in the early treatment of burns: A pilot study. American Journal of Clinical Hypnosis, 26, 9-15.
Marshall, B. J., & Warren, J. R. (1984). Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet, 1, 1311.
Mason, A. A. (1952). A case of congenital ichthyosiform erythrodermia of Broq treated by hypnosis. British medical Journal(August 23), 422-423.
Mason, A. A. (1955). Octhyosis and hypnosis. British medical Journal(July 2), 57-58.
Mason, A. A., & Black, S. (1958). Allergic skin responses abolished under treatment of asthma and hayfever by hypnosis. Lancet, 877-880.
McGlashan, T. H., Evans, F. J., & Orne, M. T. (1969). The nature of hypnotic analgesia and placebo resonse to expeimental pain. Psychosomatic Medicine, 31, 227-246.
Minsky, M. (1987). The society of mind. New York: Simon & Schuster.
Moore, L. E., & Kaplan, J. Z. (1983). Hypnotically accelerated burn wound healing. American Journal of Clinical Hypnosis, 26(1), 16-19.
Neisser, U. (1967). Cognitive psychology. New York: Appleton-Century-Crofts.
Nomura, A., Stemmermann, G. N., Chyou, P.-H., Perez-Perez, G. I., & Blaser, M. J. (1994). Helicobacter pylori infection and the risk for duodenal and gastric ulceration. Annals of Internal Medicine, 120, 977-981.
Overmier, J. B., & Murison, R. (2013). Restoring psychology’s role in peptic ulcer. Applied Psychology: Health & Well-Being, in press.
Patterson, D. R., Goldberg, M. L., & Ehde, D. M. (1996). Hypnosis in the treatment of patients with severe burns. American Journal of Clinical Hypnosis, 38(3), 200-212; discussion 213.
Price, D. D., Finniss, D. G., & Benedetti, F. (2008). A comprehensive review of the placebo effect: recent advances and current thought. Annual Review of Psychology, 59, 565-590.
Rainville, P., Hofbauer, R. K., Bushnell, M. C., Duncan, G. H., & Price, D. D. (2002). Hypnosis modulates the activity in cerebral structures involved in the regulation of consciousness. Journal of Cognitive Neuroscience, 14(Suppl), 887-901.
Shapiro, A. K., & Shapiro, E. (1997). The powerful placebo: From ancient priest to modern physician. Baltimore, Md.: Johns Hopkins University press.
Spanos, N. P., Stenstrom, R. J., & Johnson, J. C. (1988). Hypnosis, placebo, and suggestion in the treatmet of warts. Psychosomatic Medicine, 50, 245-260.
Spanos, N. P., Williams, V., & Gwynn, M. I. (1990). Effects of hypnotic, placebo, and salicylic acid treatments on wart regression. Psychosomatic Medicine, 52, 109-114.
Surman, O. S., Gottlieb, S. K., Hackett, T. P., & Silverberg, E. L. (1973). Hypnosis in the treatment of warts. Archives of General Psychiatry, 28, 439-441.
Young, P. C. (1925). An experimental study of mental and physical functions in the normal and hypnotic states. American Journal of Psychology, 36, 214-232.
Young, P. C. (1926a). An experimental study of mental and physical functions in the normal and hypnotic states: additional results. American Journal of Psychology, 37, 345-356.
Young, P. C. (1926b). Hypnotism. Psychological Bulletin, 23(9), 504-523.
Young, P. C. (1927). A general review of the literature of hypnotism. Psychological Bulletin, 24, 540-560.
Young, P. C. (1931). A general review of the literature on hypnotism and suggestion. Psychological Bulletin, 28, 367-391.
This page last revised 10/02/2013.
This article can be found here: http://socrates.berkeley.edu/~kihlstrm/SCEH2013.htm